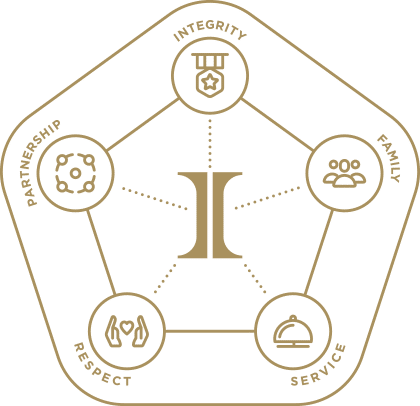
We know that by staying true to our values, we’ll never lose sight of who we are. Integrity, family, service, respect and partnership drives everything we say and do.
Insurance News

ManhattanLife’s 2024 Q1 Medicare Supplement Incentive
January 24, 2024

Unlimited Earning Potential with Aflac’s Quarter One Medicare Supplement Incentive
January 24, 2024

Wellabe Medicare Supplement’s First Quarter Incentive
January 23, 2024

Celebrate 2024 with ACE Med Supp Incentives
January 19, 2024

Access Exclusive PlanEnroll Leads This AEP
October 20, 2023

ManhattanLife’s Medicare Supplement Q4 Incentive
October 4, 2023

Lumico’s Quarter 4 Med Supp Incentive
October 3, 2023

Aflac’s Quarter 4 Medicare Supplement Incentive
October 3, 2023
ACE Med Supp Autumn Agent Incentive
October 3, 2023

LifeShield’s Quarter 4 Agent Sales Incentive Program
October 2, 2023

Medico by Wellabe’s Fourth Quarter Incentive
October 2, 2023

Ask Integrity is LIVE
September 18, 2023

Mutual of Omaha’s Broker Experience Improvements
September 15, 2023

Mutual of Omaha Enhanced Bonus Opportunity
September 5, 2023

2024 Plan Year Marketplace Registration and Training
August 2, 2023

Lumico’s Q3 Medicare Supplement Incentive
July 6, 2023

ACE Medicare Supplement Summer Agent Incentive
July 6, 2023

ManhattanLife’s Quarter Three Incentive
July 5, 2023

Medico by Wellabe’s Quarter 3 Incentive
July 5, 2023

Anthem’s 2024 Medicare Certifications
June 27, 2023

Aetna’s 2024 Medicare Producer Certification
June 27, 2023

Consumer Consent and Eligibility Application Requirements
June 15, 2023

2024 AHIP Available on June 21, 2023
June 2, 2023

Lumico’s Quarter 2 Med Supp Incentive
April 5, 2023

ManhattanLife Spring Med Supp Incentive
April 5, 2023

Medico’s Q2 Cross-Selling Extravaganza
April 5, 2023

Medico’s Quarter 2 Agent Med Supp Incentive
April 5, 2023
